Q&A with Narativ CEO, Jerome Deroy
Healthcare is a hot topic and one of the chronic issues that exists within the industry today is around improving access and inclusion to quality patient care for everyone. Providing this access often depends on securing enough funding, which relies heavily on convincing legislators to approve those funds. However, these initiatives are not always immediately appealing to legislators, so it can be very important for accessible healthcare providers to present these matters in a way that demonstrates impact. This is where the ability to tell a powerful story makes all the difference.
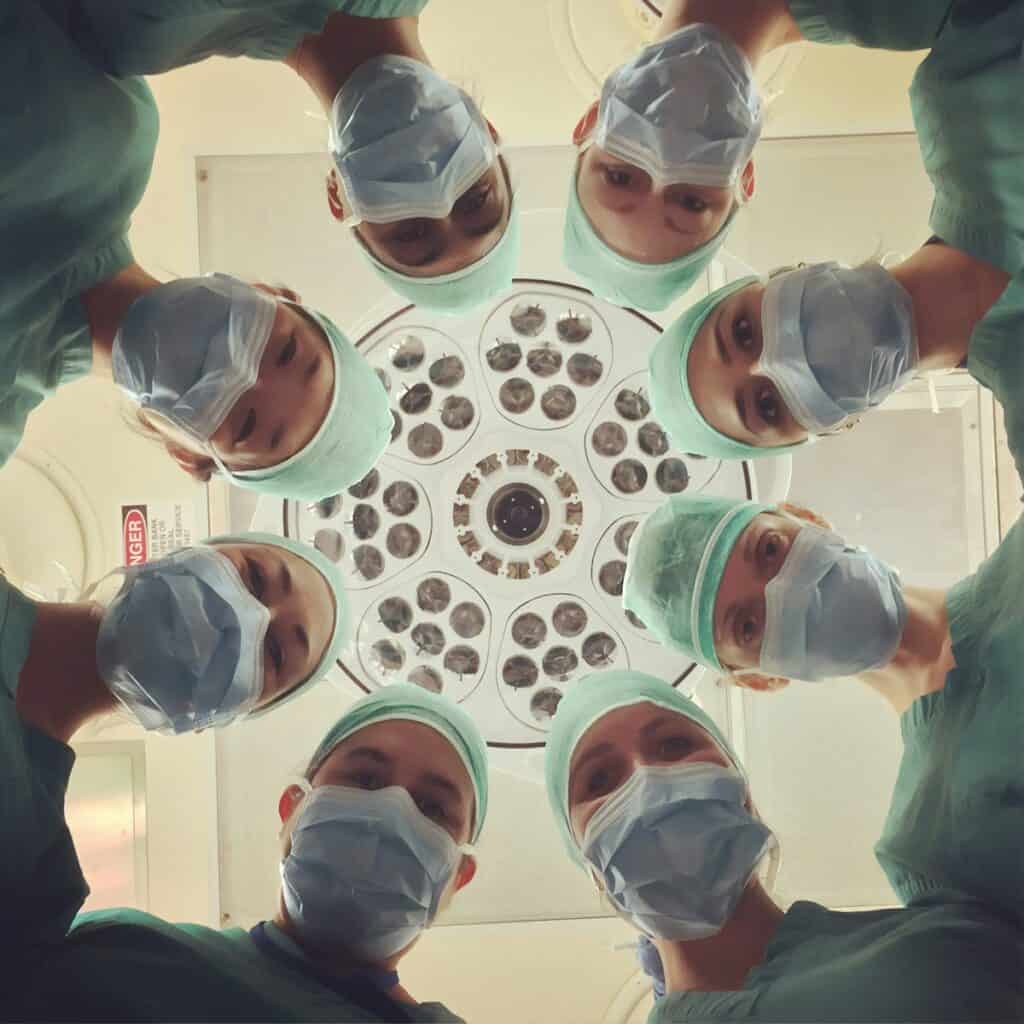
Narativ CEO Jerome Deroy recently ran a storytelling workshop for the Texas Association of Community Health Centers (TACHC) with a focus on advocating for better access and inclusion in patient care. And so, we interviewed our own CEO about his experience during that workshop and some of the stories that came out of it. As a storytelling expert, Jerome offered insight into how stories can best be leveraged to improve the healthcare space. Here is our conversation.
There’s a lot of talk within healthcare about the importance of access and inclusion in patient care. What does that mean to you and what role do you see storytelling playing in achieving those goals?
Jerome Deroy: I think you have to go back to the origins of Narativ because this methodology of storytelling was born before the company was even incorporated. It began as simply a method to help people tell stories. This was at the peak of the HIV/AIDS epidemic, and the people it was intended to help were highly marginalized without access to the care they needed. People were dying, and there were no treatments like those that exist today.
It’s in that context that our founder, Murray Nossel—who was a social worker at the time—started having people tell their stories as a way to advocate for themselves and gain access to better care.
What we do now has really not deviated much from that original beginning. We look to help people who are on the margins get better access to care through the use of personal stories.
It sounds like there were several stories developed for the TACHC workshop. What was the goal in telling these particular stories?
JD: That’s a good transition from what I was just talking about because now, 30 years later, here I was in Texas, speaking at a conference for the Texas Association of Community Healthcare Centers.
As you talk to these community healthcare centers you’ll notice they all have certain kinds of words as their values. They’ll have equity; they’ll have access; they’ll have justice. What I wanted to do was to understand these words and their values.
This conference took place in Austin, Texas, and the next day, all of the people participating in the conference were going to the capital to talk with legislators as they worked toward getting a number of initiatives funded. To prepare them for that, I wanted to have several attendees share stories that could be representative of the universal values all these health centers hold. The goal was to present the story at the conference and inspire others to tell stories of their own similar experiences—because, ultimately, telling inspiring stories like this enables you to start a relationship with someone. And that’s what all of these centers needed to do with legislators the next day.
How were these stories excavated? If someone else wants to do this for themselves, how do they go about doing that?
JD: I helped Mikki, a community health center CEO, and John, a board member and patient at a different community health center, develop the stories we shared at the conference. With both of them, we started with listening. I began by just listening to them without talking about stories. I asked them to think about some experiences they could connect to the most important value they hold dear—something that represents what their community health center is about.
Both of them talked about access and inclusion, they talked about universal care, and they talked about equity. Once we had those values, I asked them, “Can you think of an experience you’ve had in the context of your work with the health center that would bring this value to life?”
In my mind, this is where the storytelling mechanism starts.
As I’m listening to somebody tell me about an experience, I’m asking a question as they tell me about it, and my question really boils down to two words: what happened?
So, for instance, Mikki was starting to tell me, “Well, we had someone who came to our health facility and they were really in a bad way. Everyone else had refused them, and they’d been in and out of facilities. There was a lot of trauma.”
And I said, “Could you just tell me exactly what happened to this person when they walked into your facility? Did somebody come to them and ask them questions that brought out everything that you’re telling me?”
That’s when she told me about these three key personnel who worked with this individual at different stages. That’s when the word “trauma” became “Well, actually he had old gunshot wounds, and he’s been in and out of prison, and he doesn’t know how to read and write.”
So I got a lot more details from asking, “Can you just tell me what happened the moment that person walked in?” With that question I started to get a story rather than hearing what someone thought or felt about the situation. By focusing on “what happened?” we were able to uncover more details.
For example, you don’t have to tell me you were sad or upset. I can intuit that for myself. It’s so much more satisfying as a reader, a viewer, a listener, to be able to have that feeling myself—and with that, now I’m emotionally invested because I’m feeling emotions too.
What advice would you offer organizations or healthcare professionals who are trying to encourage storytelling in patient care?
JD: It really does have to begin with the values. What values do you espouse, and are you able to look through your organization and make sure the people who have the stories that can bring these values to life are being heard and are given a way to tell those stories?
It starts with having someone who’s actually listening to people who can bring these values to life. You’re listening for stories and then giving the storyteller some of the principles I’ve talked about here and in other resources, where essentially you’re sitting down with someone and you’re listening to them and you’re asking them questions to pull out the story.
And the guiding light is always that overarching value. What’s that core value that you need to go after and find stories for so other people are going to believe you when you say that’s your organization’s north star?
Do you have any final insights you would like to add?
JD: I think there are so many different dynamics and players in the healthcare system that your message can easily get lost if you’re trying to tell a story that’s going to hit all of these audiences. This makes it important to guard against the impulse to try to be everything for everyone.
I tell people to trust that one story can make a difference but to know it’s not necessarily going to be the story that everyone loves and signs up for.
You’re going to have to create more stories for different kinds of audiences. You’re going to have to think about your audiences in a new way, but if you don’t start somewhere, you’ll never start. There’s no one story that’s going to be the silver bullet for all your audiences—but each can make an impact.
Thank you Jerome for sharing your insights on how to leverage stories to improve patient access and inclusion in the world of healthcare! It is our hope that as more people are encouraged to identify and share their own stories we can reach a future where quality healthcare is truly accessible to everyone.
If you would like to learn more about how storytelling can help to improve your workplace and the world around you, you can visit us here or schedule a consult with our CEO, Jerome Deroy.